What is menopause? Signs, Stages, Symptoms & Treatment of menopause
What is Menopause?
Many people toss around the term “Menopause” comfortably and casually as if they have a thorough understanding of the life transition that is widely known as “The Change”. For starters, let’s get our terminology straight. This will be helpful moving forward. And then we’ll unpack the most common characteristics of this stage of a woman’s life and try to answer the most daunting questions that arise.
Let’s carefully define the familiar term “menopause” in a way that distinguishes it from the lesser known term “perimenopause”. Often, people (and even some healthcare professionals) refer to everything women are facing as they go through this transition (the hot flashes, sleep struggles, mood swings, etc.) as “menopause”. But “menopause” actually refers to that one day in a woman’s life when she reaches one year after the first day of her last bleed. From then on, she is considered “postmenopausal”. And “perimenopause” refers to the long and varied time of physical changes until the end of blood flow. So now that we have our terminology straight, let’s delve in!
When does Menopause start, and how long does it last?
Remember that we are actually talking about perimenopause here. The average age of crossing from perimenopause into menopause is 51. Some women simply stop bleeding and that’s the end. Plain and simple. Other women experience a roaring of unpredictable surges of symptoms that can last a long time… 1 to 3 years, or maybe more. These women experience dramatic shifts in the amounts and frequency of bleeding over many months or even years. And it’s during this storm that a brand new depth of healing is to be explored. It’s impossible to predict how any one woman’s experience will unfold! Perimenopausal symptoms may begin as early as age 35 and end as late as age 59. Symptoms may begin prematurely from some women. When a woman reaches menopause before age 40, this is considered premature menopause. Read about Early Menopause here.
I like to think of menopause as a right of passage, a concept that we are missing in today’s society. It is a time from moving from fertility into a time of letting go and shifting your perspective into that of a wiser woman. That being said, the perimenopausal shift or storm season can be grueling. Especially if you are in the space as many women: Caring for your elderly parents and adult children, or caring for your elderly parents and balancing a career.
The Centre for Menstrual Cycle and Ovulation Research states that women can actually be in perimenopause even when their cycles are still regular and normal in length. To make this unpredictable time of life a little clearer see below for a helpful table from the Centre that is widely used when trying to “diagnose” a particular woman’s stage of menopause.
Figure from The Centre for Menstrual Cycle and Ovulation Research, 2020
Women of midlife age who are still having regular cycles 21-35 days apart may still be in “Very Early Perimenopause” if they deal with any 3 of these:
Table from The Centre for Menstrual Cycle and Ovulation Research, 2020
About 80% of perimenopausal women will have hot flashes. Some will experience this while they are still having regular periods. For these women, hot flashes commonly occur right before a bleed. This “Very Early Perimenopause” stage can range from 2-5 years. I like to call these power surges 😉 Hot flashes is one of the few symptoms I see equally associated with your stress hormone cortisol and sex hormones estrogen/progesterone.
“Early Menopausal Transition”
The fun can really begin during this phase, defined by when your period becomes irregular (in cycle length/volume of blood). You can skip a month to three months between bleeds, and even though you skip a bleed, your hormones still fluctuate enough to make your mood shift, yet there is no pressure relief of the bleed.
“Very Late Perimenopause”
The final phase.If you bleed before this year is up; well, you have to start the clock all over again, unfortunately. AND, not all women pass through each phase linearly. In theory, you could go 7 months without a bleed, and then bleed again for 3 or 4 months! In Dr. Cope’s Menopause group plans, you can find great resources for tracking as your transition becomes smoother and more supported. As you can imagine, tracking through traditional period apps is not the way with the erraticism of hormones during perimenopause. To learn more about menopause group options, click here to schedule an initial visit.
What is actually happening as a woman reaches menopause?
Brain-Ovarian Connection
Physiologically, the pituitary, one of the mother hormonal glands in the brain, begins to signal to the ovaries to slow down the production of estrogen. The stories that we hear about perimenopausal “surges” are due to communication loops between ovaries and the brain. As the ovarian reserve begins to decline, the granulosa cells (in the ovaries) have less estrogen to produce. As estrogen levels decline in the body, the pituitary begins to scream to the ovaries to wake the eff up. A sudden surge of estrogen may appear and then decline and appear again, which can cause an array of symptoms. Many of these symptoms are unpredictable, seemingly random, and make it very difficult to track.
Estrogen: The Juicy Hormone
Estrogen is the hormone that gives us women our juiciness. Estrogen is responsible for healthy supple tissue; soft skin, supple vaginal tissue, cervical mucus, healthy brain function, and healthy elasticity of muscles and ligaments. Without estrogen, we can dry up. Estrogen is one reason why women are often naturally more flexible than men. When the pituitary ovarian connection results in a decline of estrogen, perimenopause enters. Though many symptoms point to an estrogen connection, it is important to scan for whole health. Often, I see many women that have imbalanced cortisol, emotional health issues, thyroiditis, low progesterone, and stealth infections that are magnified by perimenopause.
Progesterone: Mood + Sleep + More
Progesterone, another female hormone, decreases as you get closer to menopause. This happens because your body only makes progesterone if you ovulate (release an egg). As menopause approaches, you ovulate less often (or sometimes even multiple times a month!). Your progesterone level decreases. Makes sense, doesn’t it?
The Truth of your Hormones During this Time
But do you want to know something that most women’s healthcare providers don’t seem to fully grasp? I’ll let you in on the secret…so there’s this idea that for women is perimenopause, estrogen is on a continual downhill slide. Well that’s a myth. The truth is that during this time, your hormone estrogen levels can go up. “High estrogen levels, coupled with characteristically intermittent ovulation, can explain much of the misery of perimenopause” (The Centre for Ovulation and Menstrual Cycle Research) When estrogen levels are high relative to dropping progesterone…this is the root cause for the array of stormy symptoms!
These graphs depict the chaos that results from the unpredictable rising and falling of hormones during perimenopause. As you can see, the craziness you experience is definitely not all in your head! And if, by chance, you are someone who has discontinued the Birth Control Pill in your mid to late 40’s or has a history of bad periods/ postpartum, your perimenopausal hormone havoc will be even more dramatic.
What are the symptoms of (Peri) Menopause?
The pause I witness in perimenopause is generally from the following symptoms: lack of sleep, hot flashes, painful sex, brain fog, migraines, fatigue, and so much more. It is important to remember that our endocrine system (hormones) is a complex symphony of over 200 hormones. And if one is off key, it can throw the entire song out of tune. For instance, I often see hot flashes associated with stress levels, which is a cortisol connection.
Other menopausal symptoms may include:
- Irregular periods
- Short-term memory loss
- Weight gain (+ 10 pounds or more)
- Unstable emotions
- Elusive sense of well-being
- Loss of Libido
- Heart Palpitations
Symptoms of (peri) menopause are simply your body yelling for you to slow down and care for yourself during this time. Each pain and ailment is a signal to heal. As much as they can wreak havoc on your daily life and relationships, there are many different nutritional supplements and botanical medicines that can be your best ally.
These tools relieve symptoms for you to get through day-to-day life and for you to turn inward and ask yourself, “Okay, what is next to focus on in my healing journey?”
How is menopause tested ?
For blood testing, I use the World Health Organization values for fertility in order to evaluate whole hormone health. Basically, the lab values have a tighter range than what is accepted and used in the conventional medical system. In order to confirm menopause you want to find the FSH and Estradiol Levels reflect menopause. Basically Estradiol is low and FSH is way elevated. The importance of using functional medicine values for fertility is not to assess ovarian decline at the time, but also to assess for thyroid hormone and other hormones. I often like to pair this with the DUTCH test for stress hormone evaluation and your hormone fluctuations over the past month.
It is also very important to note that you have other testing options that are not offered by your conventional doctor. These include functional medicine tests that can assess environmental toxicity, cortisol, free hormones, gut health, and nutrient analyses.
Functional Medicine Labs are the labs that help your Naturopathic/ Functional Medicine Doctor take you “beyond fine” in your health goals. They are proprietary tests (unapproved by the American Medical Association) that help narrow down your wellness plan and give more information that can be used to direct your health journey. One of my favourite tests to use is the DUTCH test, a dried urine hormone test. The DUTCH test not only looks at free hormones but also your levels of cortisol, the stress hormone. One of the benefits of the DUTCH test is that it also looks at hormone metabolites. This type of testing gives us so much more information than a simple blood test for LH (Luteinizing Hormone) and FSH (Follicle-Stimulating Hormone), the two hormones traditionally measured to determine how close a woman is to reaching the cessation of her cycle.
How do we reduce Menopausal symptoms?
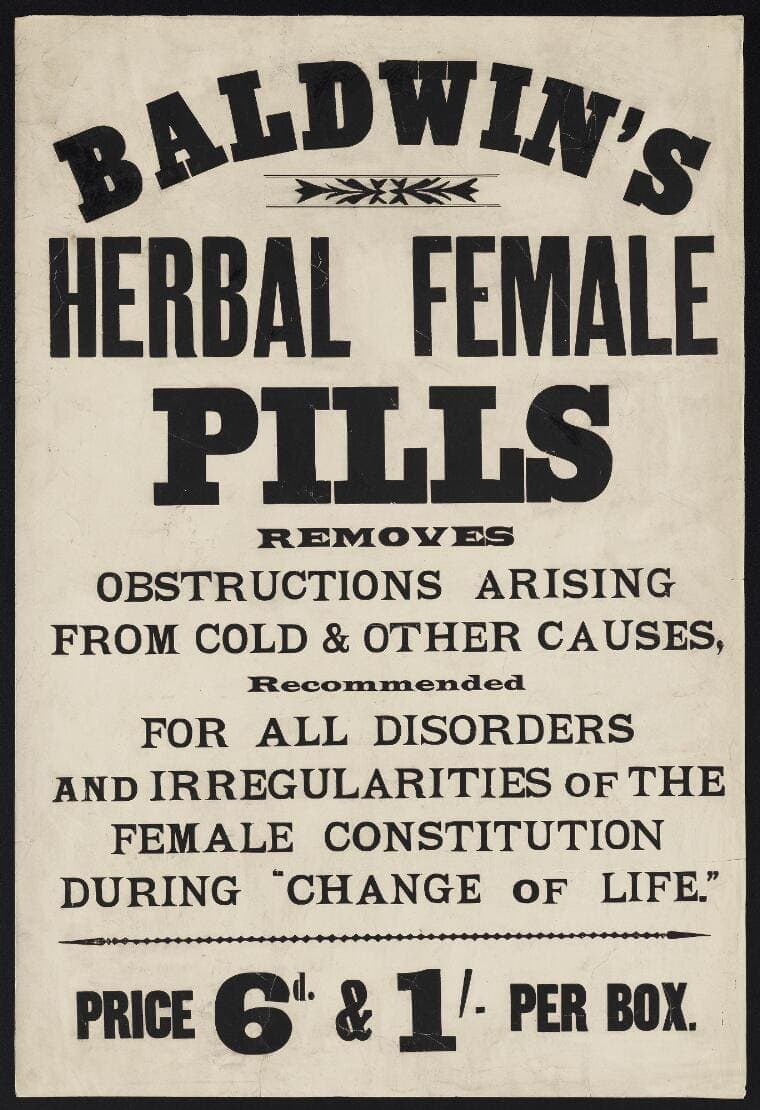
Often in conventional medicine, more extreme solutions are advised such as hysterectomies and heavy hormone replacements. Hormone Replacement Therapy (HRT) is an option, though there are many botanical remedies that are well-studied to be just as effective as HRT in managing perimenopausal symptoms.
The most common procedure I see in standard American medicine is an ablation, which is a surgical procedure that destroys the lining of the uterus to stop periods.
I have seen hysterectomies decline in the past five years. Commonly, women are told to begin (or continue) hormonal contraception (birth control) in order to control their bleeding. A birth control period is not a true period. Hormonal contraception decreases the amount of progesterone in your body, which is a protective hormone that often helps decrease symptoms of perimenopause. Bioidentical progesterone does not cause as many side effects and is a great alternative option used by naturopathic and functional medicine doctors. Bioidentical progesterone reduces heavy bleeding, eliminates hot flashes, and improves sleep.
Whereas hormonal contraception and the Pfizer-manufactured drug used to treat hot flashes, Duavee, increases the risk of endometrial cancer and other cancers.
Herbal Remedies for treatment of Menopausal Symptoms
HPA axis balancing herbs focus on cortisol and stress responses and are key during the menopausal transition. A few of my favorites are tulsi, motherwort, milky oats, and rose.
A combination of sage, rose, and milky oats is my magical blend for hot flashes.
Black cohosh, vitex, maca, and red clover, along with liver cleansing herbs, are essential to balance estrogen and progesterone. Each of these herbs support healthy hormone levels from your brain to your ovaries. I have formulated a special herbal tincture created to empower your hormone healing during this delicate life phase. I have a great perimenopause tincture available for anyone, those who joins my group menopause membership get free custom formulated tinctures.
Research is often conducted on these herbs, but is not funded because there is no fiscal value to discovering medicines that grow in your backyard! Medicines from the earth are often difficult to patent in order to reserve Indigenous rights, our original medicine people. However, a few notable studies have been done on black cohosh.
Black cohosh has been found to be as effective at relieving perimenopausal symptoms as Hormone Replacement Therapy (HRT). One study of 60 menopausal women showed black cohosh improved psychological symptoms significantly.
Another study of 60 menopausal women showed black cohosh to relieve symptoms within four weeks and cause no side effects. Both of these controlled, clinical trials showed black cohosh to be as effective as pharmaceutical estrogen. To learn more about how herbs are used to manage menopausal symptoms, read here.
Diet and Exercise during Perimenopause
Eating healthy decreases inflammation, which is important as progesterone levels go down! Ensure you are consuming healthy food daily, which means plant-based and whole foods, and organic when possible. Half of your plate should be vegetables. The rest, is protein and a starch. I have seen symptoms decrease with a simple shift to an anti-inflammatory diet. Depending on your food intolerances, this could mean cutting dairy, gluten, eggs, and or pork out of your kitchen. Remove those along with sugar and refined carbohydrates for three weeks and reintroduce one food off that list a week. Take note. Read here about the best diet for menopause.
The best exercise? The one you enjoy! However, bone density-building exercises are particularly helpful, which include weight lifting, limiting HIIT to 2-3 days a week, and pilates.
The Two Biggies: Sex and Sleep
Treating vaginal dryness
Unfortunately, one of the most devastating parts of moving into menopause is that you can finally have sex without the worry of an unplanned pregnancy, yet your vaginal tissue thins and your cervical mucous lessens, so sex is just not as enjoyable.
Also, because the tissues are thinner, friction during sex can cause bacteria to adhere to vaginal walls and make you more susceptible to urinary tract infections. Vaginal steaming is an old practice that helps bring blood flow to deliver healing cells to your lady bits. Also, the aromatics released from herbs deliver medicine directly to your tissues.
My favorite suppositories for lubrication are Bezwecken DHEA Suppositories. These soothing cocoa butter-based inserts not only help tissue moisture but also assist your adrenal glands in testosterone and cortisol production. I often recommend CBD-based lubricants to my clients, as CBD is well-researched to amplify orgasms.
Another is the O-shot, a recent procedure developed by the same doctor who founded the Vampire Facial. Platelet Rich Plasma (PRP) helps regenerate tissues when injected into joints or other areas of the body. With the O-shot, PRP is injected into the G-Spot and has been one of the most profound treatments I have witnessed for incontinence and orgasms.
And finally, the more that you have sex, the more tissue turnover in your vaginal canal, therefore you will enjoy sex more because your vaginal wall is not too thin or dry to take penetration! To read about one of my perimenopausal patient’s experience with treatments for vaginal dryness, read here.
Improving Sleep Hygiene
Sleep becomes elusive as we age. If night sweats are your ailments, I suggest keeping a sage and rose tincture and a lovely fan. Bamboo sheets may become your favorite linens. Try to get to sleep by 10 PM and stop screen time by 8 PM, as blue light interferes with melatonin, the sleep hormone. If you are having issues falling asleep, get up, listen to an audiobook, and try again. Sometimes I recommend oral progesterone. Many women in my menopause group healing class revere oral progesterone and or my menopause sleep tincture, literally revere it. 😉
Is there any help for my uncontrollable emotions?
Good news… yes there is! I offer Somatic Experiencing as an alternative therapy to help you relieve stress and integrate trauma. There are physiological reasons why stress is harder to manage during perimenopause… the estrogen receptors in the amygdala are more dense than anywhere else in our body. So when estrogen levels fluctuate, there is less consistent regulation by the prefrontal cortex. This can cause an overwhelming and disproportionate stress response; one that leaves us asking, “Why was I that upset over what happened?”
SE focuses on the mind-body connection in order to address both mental and physical concerns. The focus of SE is to help you complete processing experiences, notice the mind-body connection and cultivate awareness until you have enough capacity to work through distressing situations. Read this article to learn more information about SE which includes a patient’s perspective on this form of therapy.
Perimenopause as a Rite of Passage
In perimenopausal years, women walk through a rite of passage. There is freedom to find as monthly cycles come to an end.
Any cycling woman knows how dramatically different you feel day to day according to your hormonal cycle (and moon cycle). When that ends, you have a chance to open into a wise woman role. To hear about one of my long-time patient’s perimenopausal reflections, read here.
This does not diminish the perimenopause experience that I witness in my clients. Each woman has a unique experience of symptoms and emotional growth. I would be honored to support you on your sacred journey.
Summary
What we often call menopause is actually perimenopause.
Food matters and dramatically affects the symptoms you are experiencing during (peri) menopause.
Herbal medicines and bio-identical hormones are a less invasive and safer option with less side effects to ablation, hormonal contraception, hysterectomies, and other conventional options.
Don’t forget to enjoy sex! The more you have it, the more preserved your vaginal health will be. Lubrication, herbs, and other hacks are available to you and deeply discussed in the menopause support group. Perimenopause is a righteous passage, a new life gateway. Though it is not easy, it is a freeing entry into a wiser, newer you.
If you or someone you know is struggling with this transition, I assure you it is the best “worst” gift ever. The healing that can be harvested during this time can go as deep as you are ready. Finding a holistic practitioner who can order hormone tests, prescribe progesterone (and estrogen if necessary), and give nutritional guidance is key.